An autoimmune disease occurs when your body’s immune system attacks healthy cells within the body. This dysfunctional immune response may lead to various symptoms, like hair loss, skin rash, or even joint pain. When the body mistakenly targets skin cells, you may develop an uncomfortable or concerning rash.
I work with patients suffering from autoimmune diseases on a daily basis. Because 5-8% of Americans are likely to experience an autoimmune skin disorder at some point and women are especially at risk (thanks, genetics), I find that it’s easiest to inspect a rash a patient presents with to determine what’s behind it.
The most common autoimmune diseases that may cause rashes include:
- Psoriasis
- Eczema
- Lupus
- Sjogren’s syndrome
- Dermatomyositis
- Hypothyroidism & myxedema
- Celiac disease
- Scleroderma
- Lichen planus
- Behçet’s disease
What Does an Autoimmune Rash Feel Like?
Some of the symptoms most common to autoimmune rashes are:
- Inflamed, red skin: Like with any rash, your skin may turn red or otherwise discolored (some autoimmune rashes are more purple or brown in color) and feel warmer than the surrounding skin.
- Itch: Some, though not all, rashes associated with autoimmune disease cause an urge to itch.
- Pain or discomfort: Some rashes may hurt or feel tender when touched, while others may cause persistent discomfort.
- Varied shapes, sizes, and rash patterns: If you have an autoimmune rash, you may observe its size or shape change. Rash patterns vary and may also morph over time.
What Causes an Autoimmune Rash?
Various types of autoimmune activity may cause any number of rashes. There are several factors that may lead to autoimmune disease and dysregulated immune responses, such as:
- Genetics: Like many conditions, a genetic predisposition to autoimmune disease increases the likelihood you will develop autoimmunity. The more blood relatives you have who suffer from these diseases, the higher your chances will be.
- Hormones: Your hormonal makeup impacts the way your immune system functions. Major changes to hormone levels, like those that occur during menopause and pregnancy, can trigger autoimmunity and related skin rashes. That’s one reason females are more likely than males to have autoimmune issues.
- Mental health: Particularly if you already have an autoimmune condition, anxiety, stress, or other mental health concerns may trigger flare-ups. Your gut and brain are closely connected, so significant changes to your mental health or nervous system function play a part in autoimmune responses.
- Environmental triggers: If you’re sensitive to certain chemicals in everyday items such as detergent, body wash, or makeup, these chemicals may increase your likelihood of developing an autoimmune rash.
Let’s take a look at the specific autoimmune conditions that are most likely to cause a rash and how these rashes may present.
Psoriasis


Psoriasis is the most common autoimmune skin rash, presenting as scaly, dry, and often red skin. Psoriasis can show up anywhere on the body but most commonly affects the elbows, knees, lower back, and scalp. It’s likely to cause itching and pain or sensitivity to the touch. As much as possible, avoid scratching these patches of scaly skin, which may cause bleeding and lead to infection.
Eczema

Eczema is an itchy skin condition that affects children more than adults. Though eczema often goes away after puberty, it can persist into adulthood. Some eczema attacks are contact dermatitis, caused by exposure to a chemical irritant or an allergic reaction. However, the most common form of eczema is atopic dermatitis, caused by genetics and/or autoimmune disease. Many people experience atopic dermatitis, asthma, and hay fever together.
If you have eczema, you may experience rashes all over your body, especially on the hands, feet, arms, legs, elbow, knees, scalp, and the back of the neck.
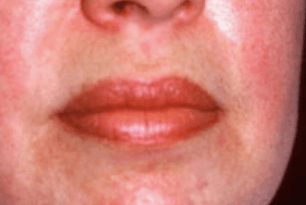
Lupus

Among other symptoms, two-thirds of lupus patients will develop a skin condition. Skin disease in lupus may present as rashes, sores, lesions, or cherry angiomas — a bright red, raised patch of skin. Up to 70% of lupus cases are worsened by sun exposure or extended time under fluorescent lights. Many lupus-related rashes will appear in sun-exposed areas of the skin, often a butterfly-shaped rash across the nose and cheeks.
Cutaneous lupus refers to a form of lupus that only affects the skin. (When people say “lupus,” they’re usually talking about systemic lupus erythematosus (SLE), which is different from cutaneous lupus.) You can have multiple forms of lupus or only one form.
Neonatal lupus is a very rare condition that affects infants of mothers who have some form of lupus. At birth, the infant may exhibit a skin rash, low blood cell count, liver problems, or a slow heartbeat.
[bravepop id=”42715″ align=”center”]
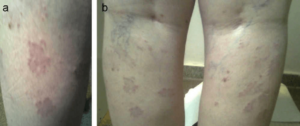
Sjögren’s Syndrome
Sjögren’s syndrome is an autoimmune disease that most frequently causes dry eyes and dry mouth. It’s most common in women over the age of 40, and it can cause multiple skin problems, such as:
- Dry, rough skin (AKA xerosis)
- Blood spots on your legs (AKA purpura) due to blood vessel inflammation (AKA vasculitis)
- Purple-to-red skin rash that does not lighten under pressure
- Red, ring-shaped skin lesions around a pale center (AKA annular erythema)
If you experience purpura or annular erythema, schedule a visit with your doctor or dermatologist right away.
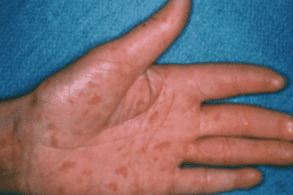
Dermatomyositis
Dermatomyositis is a very rare autoimmune disorder that can cause:
- Red or purple skin rash on a sun-exposed area
- Calcium deposits underneath your skin (AKA calcinosis)
- Inflammation around your fingernails
- Muscle weakness
- Trouble swallowing (AKA dysphagia)
- Difficulty talking
- Fatigue
Dermatomyositis-related skin rashes most often occur in these 8 parts of the body:
- Eyelids
- Nose
- Cheeks
- Back
- Upper chest
- Elbows
- Knees
- Knuckles
Individuals who experience skin rash but not muscle weakness likely suffer from amyopathic dermatomyositis, also called “dermatomyositis sine myositis.”
Read Next: What Is Methylene Blue?
Hypothyroidism & Myxedema
Severe, untreated hypothyroidism may lead to myxedema, which either means “severely advanced hypothyroidism” or skin problems related to severely advanced hypothyroidism. Myxedema leads to skin changes, though these may not technically be considered rashes. Myxedema may result in swelling and thickening of your skin.
Myxedema and severe hypothyroidism require immediate treatment and management. “Myxedema crisis” is when the body no longer tolerates the severe hypothyroidism symptoms. Your body starts to shut down. Myxedema crisis may result in coma, seizures, and death.
Call your doctor or emergency services immediately if you believe you’re having a myxedema crisis.
Celiac Disease

Although celiac disease most frequently triggers gastrointestinal distress, it can also trigger an autoimmune rash called “dermatitis herpetiformis”, an itchy, blistering rash on your skin. This usually appears on the elbows, knees, or buttocks.
Fewer than 10% of individuals with celiac experience both skin problems and the more common digestive symptoms. More often than not, patients have only one or the other.
Scleroderma
Also known as systemic sclerosis, scleroderma is a condition in which your immune system mistakenly attacks your own healthy tissues, namely, the skin. When you have scleroderma, your skin changes in appearance and feel, due to increased collagen production. It may become shiny and thicker.
Morphea is sometimes synonymous with scleroderma, but morphea is actually a severe type of scleroderma. Morphea specifically refers to oval-shaped areas of thick, red skin.
Lichen Planus
Oral lichen planus is an autoimmune disease that may trigger swelling and irritation on your skin, scalp, nails, genitals, and mucous membranes. Lichen planus typically causes purple, itchy, flat bumps on the skin. It may also result in lacy-white lesions in the mouth.
Behçet’s disease

Behçet’s disease is a very rare autoimmune disorder that leads to blood vessel inflammation (vasculitis).
Autoimmune Blistering Diseases
We’ve been talking a lot about skin rashes. However, some autoimmune conditions can cause skin blistering, too.
Also known as autoimmune bullous diseases, the most common autoimmune diseases that can cause blistering are:
- Epidermolysis bullosa acquisita
- IgA-mediated bullous dermatoses
- Ocular cicatricial pemphigoid
- Bullous pemphigoid
- Pemphigus
When to Call Your Doctor
It’s always advisable to keep an eye on a new rash. Here are some signs that you should see a healthcare professional:
- Sudden onset of a new rash
- Fever
- Pain
- Blisters
- Swelling
- Discharge
- Bruising
- A bad smell
- The rash area is spreading
FAQs
If you have questions about rashes and autoimmune diseases, you’re not alone. Here are some commonly asked questions:
What autoimmune diseases cause an itchy rash?
Several autoimmune diseases can cause itchy rashes, like lupus, Sjögren’s syndrome, dermatomyositis, lichen planus, and dermatitis herpetiformis (linked to celiac disease). These conditions make the immune system attack the skin, leading to itchy and uncomfortable rashes.
Certain conditions are also known for causing scalp itch, including:
- Psoriasis
- Eczema
- Lichen planus
- Lupus
- Scleroderma
- Sjögren’s syndrome
Why do autoimmune conditions cause a rash?
Autoimmune conditions can cause a rash because the immune system mistakenly attacks healthy skin cells. This leads to inflammation, redness, and irritation. Basically, the body’s defense system goes a bit haywire and targets the skin, causing those itchy and visible symptoms.
How long does an autoimmune rash last?
Autoimmune diseases and skin rashes can last a different amount of time depending on what’s causing them and how well they respond to treatment. Some can stick around for months or even become chronic, while others get better quickly with the right care. Working with an experienced integrative medicine team such as PrimeHealth Denver allows you to explore all possible causes to get the right diagnosis while treating you holistically.
What do autoimmune rashes look like?
Rashes and autoimmune disorders can show up in all sorts of ways, depending on the condition. You might see red or purple patches, itchy flat bumps, ring-shaped spots, or even blisters. For example, lupus often causes a butterfly-shaped rash across the nose and cheeks. On the other hand, Sjögren’s syndrome can lead to dry, rough skin and tiny blood spots. It’s amazing how varied these rashes can be!
What autoimmune conditions may cause hives?
Autoimmune hives are itchy red bumps or welts often caused by allergic reactions. An overactive immune system can also cause them. Autoimmune diseases that may cause hives are:
- Lupus
- Sjögren’s
- Celiac disease
- Type 1 diabetes
- Rheumatoid arthritis
- Vitiligo
How will my doctor test for autoimmune disease?
To check for autoimmune diseases, your doctor at PrimeHealth Denver will start by asking about your medical history and doing a physical exam. They might use blood tests to look for specific antibodies or signs of inflammation. Depending on what they suspect, they could also recommend skin biopsies, imaging studies, or other specialized blood tests to confirm what’s going on and how severe it is. Always talk to your healthcare provider for advice and testing tailored to you.
Here are 4 common diagnostic tests for autoimmune disease:
- Antinuclear Antibody (ANA)
- Autoantibodies
- C-Reactive Protein (CRP)
- Erythrocyte Sedimentation Rate (ESR)
Will I need a skin biopsy? Your doctor may recommend a biopsy to learn more about a new rash. This is to rule out bacterial or fungal infections, cancer, or other skin conditions.
What to Do About Autoimmune Rashes
When dealing with autoimmune rashes—or autoimmune disorders in general—the key to effective treatment is identifying and addressing the underlying cause. Autoimmune issues can arise from a variety of factors, so it’s crucial to pinpoint exactly what’s triggering your symptoms.
For immediate relief, over-the-counter corticosteroid creams can be very helpful in reducing discomfort. These creams work by reducing inflammation and soothing the skin, making those itchy, red areas more manageable.
However, for a lasting solution, it’s important to consult with a healthcare provider who can guide you through the process. At PrimeHealth Denver, we specialize in integrative medicine, which means we look at the bigger picture, considering all possible causes of your condition. Our team conducts thorough evaluations and employs a holistic approach, aiming to treat you as a whole person, not just your symptoms.
If you’re in Colorado, come see us at PrimeHealth! We spend 1-2 hours at each appointment with our patients to thoroughly understand their unique needs and circumstances.
Diagnosing Autoimmune Rashes
Diagnosing autoimmune rashes isn’t as intimidating as it might sound. When you visit healthcare professionals like our expert team at PrimeHealth Denver, we’ll start by chatting with you about your medical history and symptoms. This helps them understand what might be causing your autoimmune rash. We’ll also closely examine your skin during a physical exam. The physical exam can reveal information such as:
- How the rash looks
- Where it is located on the body
- Whether it’s raised or flat
- If it is dry, scaly, painful, or fluid-filled
After these assessments, we will recommend blood tests and biopsies to confirm our suspicions. These diagnostic tools help us determine which autoimmune disorder you have and how severe it is. By taking this thorough approach, our team at PrimeHealth Denver ensures we get to the root of your problem, so they can help you feel better as soon as possible.
Treatment Options for Autoimmune Rashes
Dealing with autoimmune rashes can feel overwhelming, but there are many treatment options that can help manage and alleviate your symptoms. Let’s break down some of the most effective treatments available today.
Topical Creams
Topical creams, such as corticosteroids and calcineurin inhibitors, are often the first line of defense against autoimmune rashes. These creams work by reducing inflammation and suppressing the immune response in the affected area. According to a study published in the Journal of Dermatology, low-dose corticosteroids are effective in reducing the symptoms of autoimmune rashes, providing quick relief from itching and redness.
Oral Medications
If things get worse, your doctor might give you pills to help. These could be immunosuppressants like methotrexate or azathioprine to calm your overactive immune system. Antihistamines can also help with itching. A study shows that immunosuppressants help reduce the severity and frequency of rashes in chronic autoimmune conditions.
Phototherapy
Phototherapy, also known as light therapy, involves exposing your skin to ultraviolet light under medical supervision. This treatment can help slow down the rapid skin cell turnover that comes with autoimmune rashes. Research supports its effectiveness, showing that phototherapy can significantly improve skin lesions in conditions like psoriasis and eczema.
Biologic Therapies
Biologic therapies are a newer type of treatment that focuses on specific parts of the immune system. Medications like TNF inhibitors (think adalimumab and etanercept) have shown great promise in treating autoimmune rashes. A clinical trial published in Clinical Immunology highlighted the effectiveness of TNF inhibitors, showing significant improvements in patient symptoms and quality of life.
Importance of Individualized Treatment Plans
One size definitely doesn’t fit all when it comes to treating autoimmune rashes. Everyone’s condition and needs are unique, so a tailored approach is key. At PrimeHealth Denver, we take the time to thoroughly evaluate each patient to create personalized treatment plans. This way, you get the most effective and appropriate care. By looking at the severity of your symptoms, your medical history, and specific triggers, we can develop a comprehensive strategy that tackles both your immediate discomfort and your long-term health goals.
If you’re in Colorado, come see us at PrimeHealth! We spend 1-2 hours at each appointment with our patients to thoroughly understand their unique needs and circumstances.
Lifestyle Management Strategies
Managing an autoimmune rash can feel like a juggling act, but with the right lifestyle changes, you can make a world of difference in your symptoms. Let’s dive into some practical tips that have been shown to help autoimmune diseases and skin rashes.
Maintaining a Healthy Diet
Eating the right foods can significantly impact how you feel. A balanced diet rich in anti-inflammatory foods like fresh fruits, vegetables, whole grains, and lean proteins can help manage autoimmune conditions. Research suggests that an anti-inflammatory diet rich in antioxidants can reduce flare-ups and improve overall skin health.
Managing Stress Levels
We all know that stress can take a toll on our health, but it’s especially important for those dealing with autoimmune rashes. High-stress levels can exacerbate symptoms and trigger flare-ups. According to a study published in Dermatology Practical & Conceptual, stress management techniques such as mindfulness meditation, deep-breathing exercises, and yoga have been effective in reducing the severity of autoimmune symptoms. Taking 15-30 minutes a day to practice these techniques can make a noticeable difference.
Avoiding Potential Triggers
Identifying and avoiding your specific triggers is crucial for managing autoimmune rashes. Common triggers include certain foods, environmental factors like pollen or pet dander, and even weather changes. Keeping a symptom diary can help you pinpoint what might be triggering your rash so you can avoid it in the future.
Practicing Good Skincare Habits
Taking care of your skin is essential when dealing with autoimmune rashes. Using gentle, fragrance-free cleansers and moisturizers can help keep your skin hydrated and reduce irritation. According to a study, maintaining a regular skincare routine with products designed for sensitive skin can help reduce flare-ups. Also, be sure to protect your skin from the sun by using sunscreen with a high SPF, as sun exposure can worsen some autoimmune conditions.
Autoimmune Diseases and Skin Rashes: The Connection
Understanding the connection between autoimmune diseases and skin rashes is vital for managing your symptoms effectively. Each person’s journey with autoimmune conditions is unique, but by adopting individualized treatment plans, making beneficial lifestyle changes, and leaning on the support of communities, you can navigate this challenging path more smoothly.
Remember, you’re not alone in this process. At PrimeHealth Denver, we are dedicated to providing personalized, comprehensive care to help you achieve your health goals and improve your quality of life. If you’re in Colorado, don’t hesitate to reach out and take the first step towards better health today!
If you’re in Colorado, come see us at PrimeHealth! We spend 1-2 hours at each appointment with our patients to thoroughly understand their unique needs and circumstances.






