Mast Cell Activation Syndrome (MCAS) involves a spectrum of symptoms that often ebb and flow over a lifetime. It’s a result of over-activation of our mast cells, , which release chemical mediators that cause inflammation in the body.
Typically, MCAS causes a wide range of allergic and autoimmune symptoms, but many people experience more non-specific symptoms. This makes this condition challenging to recognize and leaves many sufferers without answers for years at a time.
What Are Mast Cells?
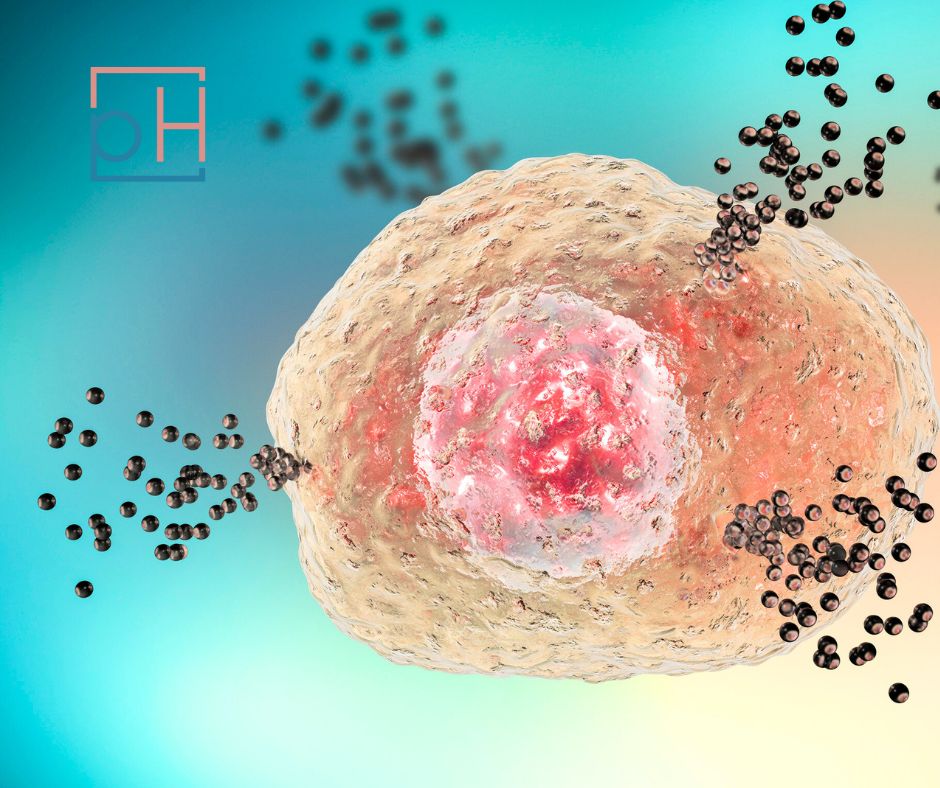
Mast cells are found throughout our body in connective tissue and organs. They are known as “allergy cells” because they are often triggered by allergens, and release mediators which cause an inflammatory cascade.
There are over 200 different chemical mediators released from mast cells. Some of the more recognizable of these include histamine and leukotrienes.
These are well-known in allergic conditions. Many medications block the effects of these chemicals, such as antihistamine allergy medications or montelukast, a common prescription used in allergies and asthma.
There are many potential mast cell triggers. Some of these include:
- Allergies
- Temperature changes
- Exercise
- Stress (emotional or physical)
- Certain foods and beverages
- Medications; such as opioids, NSAIDs, antibiotics, some local anesthetics, and contrast dyes
- Scents, perfumes, chemical and natural odors
- Infections
- Fatigue
When the mast cells become “over-activated,” there can be several triggers, making it challenging to pinpoint the exact cause of the reactions you’re experiencing.
Mast cells also tend to be found in higher concentrations in tissues that have contact with the outside environment, such as skin, lungs, and GI tract, so it can be more likely to experience symptoms relating to those areas.
What Are the Symptoms of Mast Cell Activation?
MCAS causes a wide range of symptoms that may vary from person to person. Some of the more common MCAS symptoms include:
- Allergic congestion
- Shortness of breath
- Hives/rash, skin itching, and flushing
- Hypersensitivity to fragrances and medications
- Gastrointestinal distress including food intolerances, nausea, bloating, cramping/abdominal pain
- Fatigue and/or brain fog
- Headaches
- Body and muscle aches
- General malaise (just not feeling well)
Mast cell disease can involve life-threatening complications, such as severe allergic reactions and idiopathic anaphylaxis.
How Is MCAS Diagnosed?
A typical workup for a diagnosis of MCAS includes serum testing (blood tests) for histamine, tryptase, and prostaglandin. There is also urine testing for histamine levels, and your GI doctor can evaluate for mast cell presence in the gut through an upper endoscopy scope (known as staining for mast cells).
The diagnostic criteria for this condition are generally considered to include:
- Positive serum tryptase (after repeated measurements compared with baseline levels)
- Urinary histamine metabolites (no cutoffs have been specified for MCAS yet)
Other validated markers less commonly used in clinical practice include:
- Urinary prostaglandin D2 or metabolites (only relevant when appearing with other markers)
- Urinary leukotriene E4 (only relevant when appearing with other markers)
Because most of the chemicals released by mast cells are short-lived, this can be a tricky condition to diagnose.
Unfortunately, many who fit the symptomatic picture of MCAS won’t have labs to “prove” it. It can be helpful to check lab levels during a flare when they would theoretically be much higher. Symptom history plus improvement to therapeutic options matters as well.
Read Next: It May Be Time to Rebalance Your Nervous System
The Treatment Approach to MCAS
Most of the buzz around MCAS and its umbrella of symptoms have focused on histamine. You may have heard of “histamine intolerance,” which can be classified as a subset of MCAS. However, taking antihistamines (such as Claritin or Allegra) isn’t the only solution.
MCAS is still under-recognized in most conventional medicine settings, but thankfully that’s starting to change.
When you have been diagnosed or suspected to have MCAS, you may be given medication options. Typically, these include antihistamines (allergy medications and certain acid blockers, like famotidine), leukotriene inhibitors (montelukast), and/or mast cell stabilizers, such as liquid Cromolyn or compounded ketotifen.
Additional treatment modalities may include:
- Low histamine diet
- Stress management practices
- Healing gut dysfunction (especially if there are too many histamine-producing strains of microbes)
- Identifying and managing triggers, such as toxins, mold, and/or chronic infections
- Utilizing natural solutions to stabilize mast cells
There is typically an underlying story with MCAS. It can be helpful to work with a functional medicine practitioner, such as our providers at Prime Health, who can take a deeper dive into identifying the root cause triggering your condition.
Getting to the Root Cause of MCAS
Several medical conditions have a higher prevalence of developing into MCAS. These include Ehlers-Danlos Syndrome (EDS), Postural Orthostatic Tachycardia Syndrome (POTS), and irritable bowel syndrome (IBS).
IBS is another broad term with a root-cause etiology. Sometimes, getting to the root of IBS and addressing gut health can lead to improvement in MCAS as well. SIBO and leaky gut specifically have been correlated with MCAS.
Since the COVID-19 pandemic, there has been increased recognition of MCAS. Long-COVID-19 is now known to have a component of mast cell activation, with abnormal breakdown of these cells and excessive inflammatory release. Again, getting to the root cause of this immune dysfunction and identifying potential triggers and imbalances can be instrumental in promoting long-term healing.
Work with a provider who will take the time to get to know you, not just push you out the door. PrimeHealth providers spend 1-2 hours per visit with every single patient, and we’re here to help you get the help you truly need.
View this profile on InstagramPrimeHealth (@primehealthdenver) • Instagram photos and videos
Sources
- Fong, M., & Crane, J. S. (2018). Histology, mast cells.
- Leru, P. M., Anton, V. F., Ureche, C., Zurac, S., Bratu, O., & Neagoe, C. D. (2020). Mast cell activation syndromes‑evaluation of current diagnostic criteria and laboratory tools in clinical practice. Experimental and Therapeutic Medicine, 20(3), 2348-2351.
- Sumantri, S., & Rengganis, I. (2023). Immunological dysfunction and mast cell activation syndrome in long COVID. Asia Pacific Allergy, 13(1), 50-53.